Medi-Cal, Group Care, and Alameda Alliance Wellness
The California Department of Managed Health Care (DMHC) sets regulations that establish claim settlement practices and the process for resolving claims disputes for managed care products. These regulations comply with Assembly Bill 1455 (AB1455) for claims received on or before December 31, 2025, or AB 3275 for claims received on or after January 1, 2026. This section of our website serves as a notice to inform you of your rights, responsibilities, and procedures for claim settlement and dispute submission for Alliance Medi-Cal, Group Care, and Alameda Alliance Wellness members. Unless otherwise provided herein, capitalized terms have the same meaning as set forth in Sections 1300.71 and 1300.71.38 of Title 28 of the California Code of Regulations.
For more information on AB 1455 or AB 3275, please visit California Department of Managed Health Care (DMHC).
Title 42 CFR 422.520 provides the Medicare claims processing requirements for non-contracted providers and Title 42 CFR 424.44 defines the timely claims submission guidelines for non-contracted providers.
This section includes information for Alliance providers on the following topics:
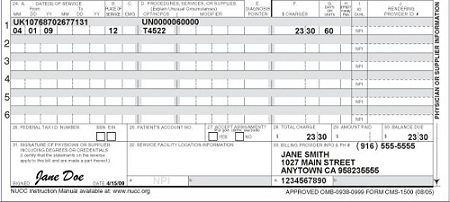
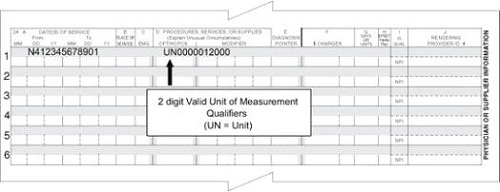
- Claim Submission Instructions
- Dispute Resolution Process for Contracted Providers
- Dispute Resolution Process for Non-Contracted Providers
- Provider Dispute Resolution (PDR) Form
- Claim Overpayments
For questions regarding claims submissions, please contact:
- Alliance Provider Services Department
- Monday - Friday, 7:30 am – 5 pm
- Phone Number: 1.510.747.4510
- Email: providerservices@alamedaalliance.org